Baba Akomolafe warns that moving care from hospitals to the community will increase pressure on GPs unless pharmacies are digitally integrated into the NHS primary care system
Pharmacists have the potential to expand Pharmacy First service, but significant barriers such as insufficient funding and digital exclusion of community pharmacies, must be addressed.
“Digitalizing needs to be done first,” said Baba Akomolafe, superintendent pharmacist at Christchurch Pharmacy, who sees the exclusion of community pharmacies from the NHS digital system as “an unnecessary bottleneck” in expanding services like Pharmacy First.
The government's elective care reform plan aims to reduce waiting times by shifting services from hospitals to community settings.
However, Baba has voiced concern that it will place more pressure on GPs unless pharmacies are digitally integrated into the NHS primary care system.
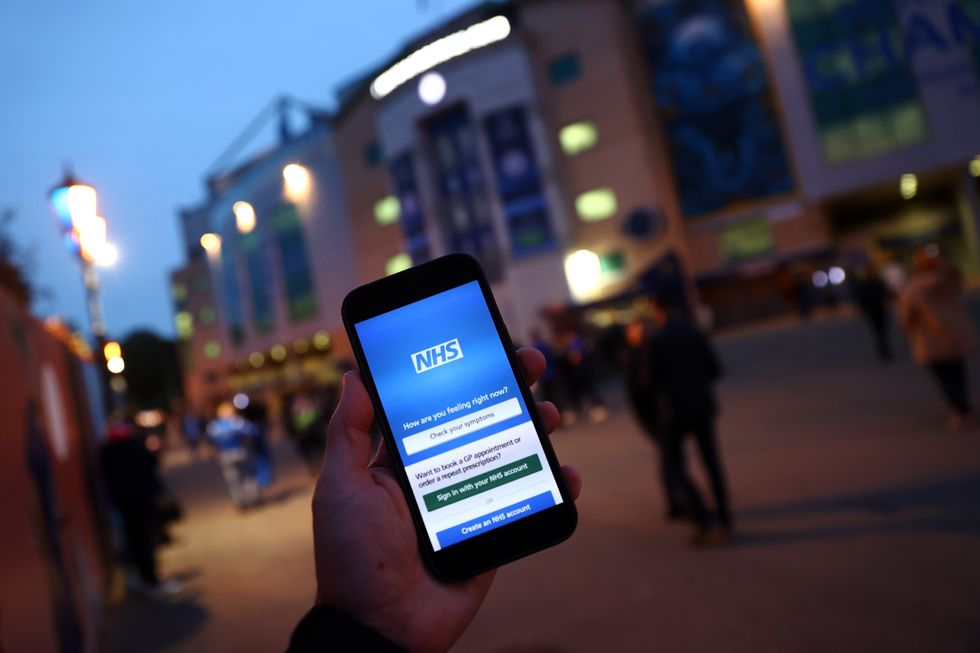
He suggested that, just as patients can communicate with their GP and book appointments via the NHS app, they should also be allowed to refer themselves to their chosen pharmacy through the app.
Speaking to Pharmacy Business, Baba argued: “What is the point of patients referring themselves to the GP digitally, and then the GP referring them to the pharmacies through an analogue system? Why doesn't the digital system give the patient the choice of pharmacies when AI could easily identify that their symptoms can be seen by a pharmacist?
He explained that if pharmacies were included in the NHS app, patients could simply search for available services like 'sore throat' and be directed to the nearest pharmacist.
Baba believes that this change would also improve awareness of available pharmacy services, ultimately benefiting both patients and healthcare providers.
"Pharmacy, as a profession, is very agile and innovative, but you can only be innovative with what’s given. If we are given the funding to innovate, we will do so.”
“When we're digitalized, GPs will feel great relief knowing their inboxes won't be filled with referrals that could have gone straight to the pharmacy. It's a win-win for everybody,” he added.
Expanding the role of pharmacies in ENT Services
When asked if the sector is ready to deliver more ENT services, as proposed in the plan, Baba said that pharmacies can and are willing to do more “as long as they are given funding to increase their capacity.”
He highlighted the success of a pilot ENT project that Christchurch Pharmacy ran between February 2023 and July 2023.
In the pilot, the pharmacy carried out earwax removal and made referrals to ENT specialists when infections were detected as they didn't have Pharmacy First at that time.
The project involved four pharmacies across Essex, including Christchurch Pharmacy, who were compensated directly by the local council for the service.
Baba pointed to the success of this initiative as evidence that pharmacies can deliver expanded Pharmacy First ENT services.
Currently, Christchurch Pharmacy provides earwax removal as a private service, treating around 1,500 patients a year.
Baba told Pharmacy Business that his pharmacy would be happy to offer this service under the NHS Pharmacy First service at a fee lower than he charges patients privately, as it did during the pilot phase, if the necessary digital infrastructure and funding are put in place.
Need to increase capacity and competence
Beyond digital integration, Baba stated that pharmacists will need to increase both their capacity and competence to take on additional roles.
This includes expanding premises to provide more consultation rooms and upskilling staff to enhance their clinical roles.
Baba also highlighted the importance of the Hub and Spoke model, which would enable pharmacies to outsource dispensing to third parties, allowing staff to focus more on clinical tasks.
However, training pharmacists to become Independent Prescribers (IPs) remains a challenge, as Baba pointed out the difficulty in finding trainers or Designated Prescribing Practitioners (DPPs) willing to mentor them.
This is particularly because experienced prescribers do not get paid to train pharmacists.
Baba said: “My staff who are willing to upgrade or upskill don't find any training opportunities.”
“Pharmacists are expected to beg experienced prescribers to accommodate them. But why would somebody train your pharmacist without getting paid?”
He called for financial incentives for trainers to help pharmacists become IPs to enable them to offer expanded services.
A call for reform
Baba's message to the government is clear: “There's no point reforming the policies without helping us to reform our practice and premises.”
Baba concluded by reiterating the need for government action on digital integration, training incentives, capacity building, and the implementation of the hub and spoke model.
.