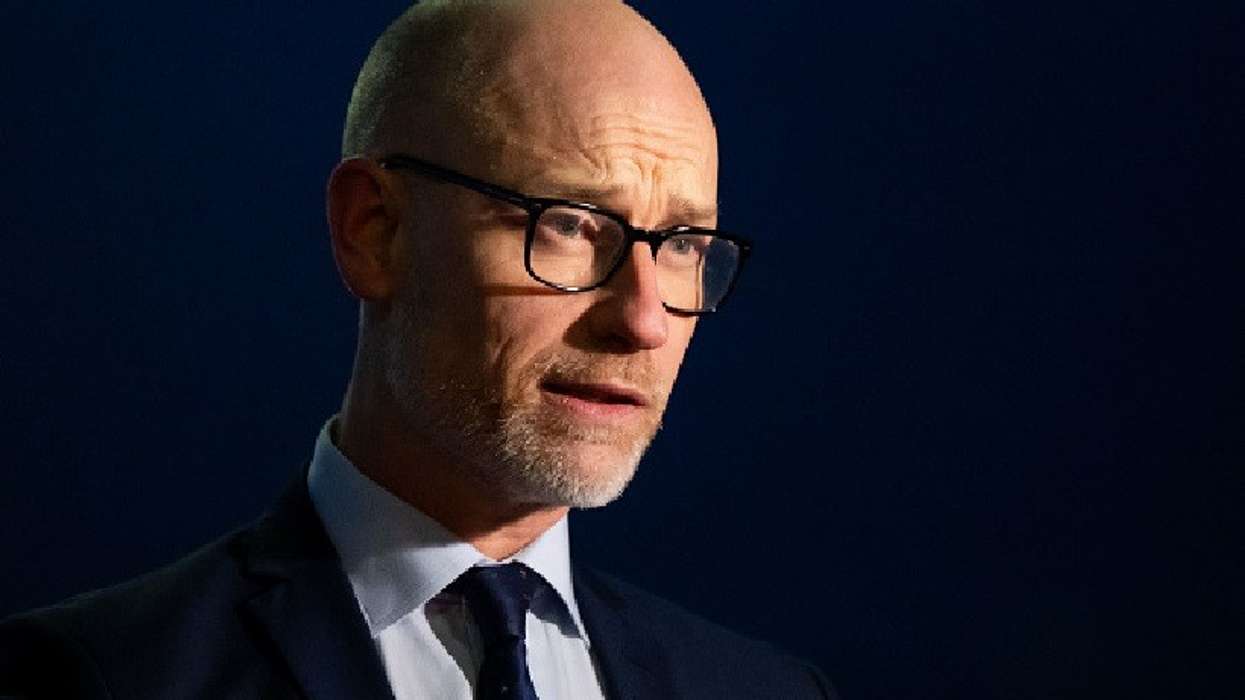
Pharmacy minister Stephen Kinnock vowed that community pharmacy will be “the cornerstone of neighbourhood healthcare” as he celebrated the very best of the sector at the annual Pharmacy Business Awards on Friday (3).
The government announced earlier this year plans for a Neighbourhood Health Service that will focus on shifting healthcare from hospital to community.
Central to the 10 Year Health Plan, the services will bring together a range of professions, including GPs, pharmacists, community nurses, hospital doctors, social care workers, dentists, optometrists, paramedics, social prescribers, local government organisations and the voluntary sector.
“The work of pharmacy teams right across the country has a key role to play in delivering our future vision for health services,” Kinnock told attendees at the 25th Pharmacy Business Awards held at the Park Plaza Hotel in central London.
“I want to see community pharmacy playing a key role in the Neighbourhood Health Service, working collaboratively with other primary care providers at to deliver the services patients need in their localities.”
Kinnock stressed the “critical role” community pharmacy plays in providing healthcare in every community, noting that 40 per cent of pharmacies are in the 30 per cent most deprived areas.
“This shows the reach into communities offered through pharmacies is second to none,” he added.
“In short, you and your teams are key to our ambition to delivering more care in the community using trusted providers.”
In March, the government approved a £3.073 billion funding package for 2025/26, along with an additional £215 million to support Pharmacy First and other Primary Care Recovery Plan services.
However, the new contract was still £2.5 billion short of the total amount the economic analysis commissioned by NHS England believed was needed for pharmacies to provide services to the public.
Whilst, not directly mentioning negotiations for the next pharmacy contract, Kinnock insisted that in just over a year in power, the government has demonstrated its commitment to community pharmacy.
“Since coming into power, we agreed a 19 per cent uplift in funding agreed - the biggest uplift across the NHS for 2024/25 and 2025/26,” he said.
“This showed our commitment to stabilising the sector and positioning community pharmacy as key players as we all work toward achieving the vision set out in the 10 Year Health Plan.”
Within the next five years, the government wants to see community pharmacies transitioning from a dispensing-led to a services-led service.
Kinnock said this plan was a reflection of how valued pharmacists are to ministers.
“Pharmacists and pharmacy technicians are highly trained professionals. I, and this government, recognise how much untapped potential there is to be able to build on the important work you all do already. I am delighted by the appetite I am regularly reminded of for innovation in this sector,” he said.
“Being here tonight and hearing about such successes makes that clear. I want to maximise the use of skills within the profession to allow pharmacists and pharmacy technicians to work the top of their licence to improve the health of the nation.
“That is why we have focused on delivering the support pharmacies need to continue to deliver for their patients to innovate and provide the care and support we all can depend on.”
Independent prescribing
The minister reiterated his commitment to introducing Independent Prescribing in community pharmacy.
From September 2026, newly qualified pharmacists will automatically become independent prescribers upon registration.
“We have seen through the successful pathfinders programmes the impact such an initiative could have. To date, 200 pathfinder sights have delivered 33,000 consultations with around 60 per cent of these resulted in a prescribing decision which would otherwise have been made in a GP or hospital,” he said.
Kinnock spoke of ongoing legislative changes that were designed to free up time for pharmacists to run more services.
He mentioned that there were discussions taking place that could see changes, such as any member of the pharmacy team to hand out a checked and bagged prescription, and pharmacists to authorise registered pharmacy technicians to lead or supervise the dispensing process and take primary responsibility for hospital aseptic facilities.
Also, last month, the Department of Health and Social Care (DHSC) launched a consultation on granting greater flexibility to pharmacists while dispensing medicines.
It will allow community pharmacists to supply a different strength or formulation (which may mean a different quantity) of the same medicine originally prescribed, in certain circumstances.
“Our aim is to allow a pharmacist to dispense an alternative product against a prescription if the exact prescribed item is not available. This will support patients and improve their experience in accessing the medicines they need – while increasing the powers of pharmacists to deliver more care in the community,” said Kinnock.
“All these measures are designed to give pharmacies greater flexibility and control in how they run their business and deploy their staff, free up pharmacists’ time to deliver more clinical services and ultimately improve patient access to medicines and healthcare services.”
Clinical services
Kinnock stressed that the future of community pharmacy was dependent on embracing clinical services.
“Looking to the future, we want to build on the fantastic range of clinical services and care you are currently offering, maximising the skills and knowledge you and your colleagues have to shift care from hospital to community and from treatment to prevention,” he said.
“I want to be clear for you all that I am in no doubt as to the value pharmacy brings to our NHS or wider society and I look forward to continuing to work with Community Pharmacy England and the pharmacy profession on what the future of pharmacy looks like.”