The NHS England(NHSE) Innovative Medicines Fund (IMF) should be efficiently utilised to expedite patient access to potentially valuable new medications, thereby incentivising the pharmaceutical industry to develop costly drugs for rare diseases, according to medical experts. However, no medicines have entered the fund since its establishment in 2021. Simon Stevens served as the Chief Executive of NHSE during that time.
In their article for the Journal of the Royal Society of Medicine, health economics and policy specialists from the London School of Hygiene & Tropical Medicine (LSHTM) cautioned that mishandling the rollout of the NHSE's IMF may deter vital evidence generation, concurrently shifting the financial onus from the pharmaceutical industry to public finances.
Expanding upon the successful UK Cancer Drugs Fund (CDF), which provided early access to critical medications for over 80,000 patients, the IMF was established with a parallel £340 million yearly budget. This fund aimed to simplify managed access agreements for treatments, including conditions like spinal muscular atrophy.
ABPI’s apprehensions on IMF
In response to the journal's report, the Association of the British Pharmaceutical Industry (ABPI) expressed concerns regarding the Fund's efficacy, particularly the requirement for drug manufacturers to bear the complete treatment costs for fund beneficiaries, even if the UK's health technology assessor subsequently does not endorse the therapy's usage.
Moreover, firms are obligated to reimburse expenses surpassing a yearly budget, the extent of which is autonomously determined by legislators.
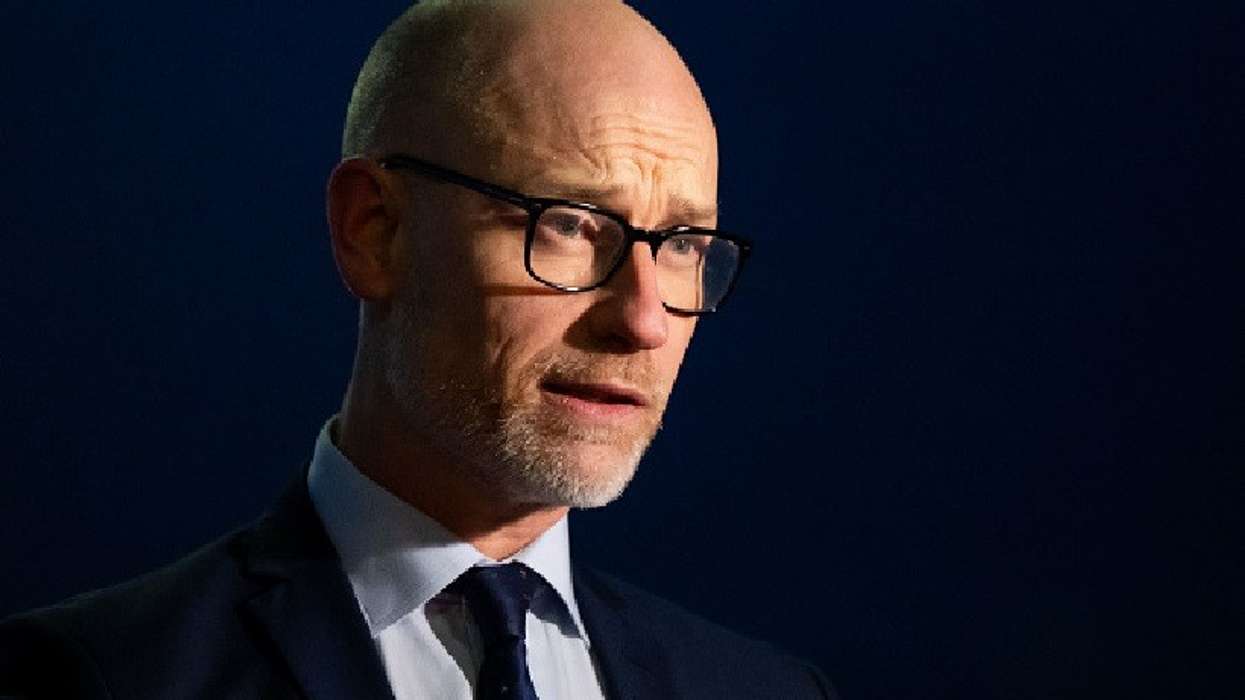
"The IMF was established over a year ago to extend managed access to new medicines for patients with various diseases, including rare conditions, while further evidence is gathered," said Paul Catchpole, Director of Value and Access Policy at the Association of the British Pharmaceutical Industry (ABPI).
"To date, no medicines have entered the fund under this premise, and we are keen to collaborate with NHS England and National Institute for Health and Care Excellence (NICE) to comprehensively comprehend the reasons and actively contribute to realising the Fund's potential for patient benefit,” he added.
Accumulated funding pool yielding limited or no results?
Since 2021, the combined funding pool for both the CDF and IMF totals £680 million (£340 million each), dedicated to expediting early access to the most promising medications. However, the experts at LSHTM contend that the CDF and IMF initiatives, acknowledged as 'managed access' schemes, are restricted solely to medications and lack extension to other forms of interventions.
They further argue that the societal value of the CDF remains unclear, highlighting concerns about the transparency of drug costs and the duration of their integration into the scheme. Similarly, the IMF's principles and operational framework are presently confined to documents, yielding restricted or negligible outcomes for NHS patients.
"Although we generally endorse the IMF's eight guiding principles, we find their operationalisation lacking adequate detail and not fully leveraging the CDF experience," said Dr Aris Angelis, Lead Author and Assistant Professor in Health Economics at the Department of Health Services Research and Policy at LSHTM.
"Addressing non-medical interventions gains specific importance in disease domains like cancer, where access to high-quality radiation and surgical treatments plays a pivotal role in enhancing outcomes," said co-author Dr Ajay Aggarwal, Associate Professor at LSHTM and Clinical Oncologist.
Critical need for precise planning
An additional concern underscored by the authors is the entry criteria for 'most promising' medicines into the IMF, which, they contend, are currently deficient in essential details.
For the IMF to effectively facilitate timely access to clinically effective, safe and cost-efficient medicines, the authors assert that meticulous design is imperative for its operational specifics and established mechanisms.
"Parallel to the CDF, the IMF should act as a pathway for patient access, also offering essential evidence—mainly from randomised controlled trials—to address uncertainties about a drug's clinical and cost-effectiveness," Dr Angelis added.
Meanwhile, the NHS reported that over 425,000 patients used its recently launched nationwide online service for completing GP registration. Operated by NHS England, this GP surgery registration service has given NHS patients efficient and easy access to registration since its launch in August 2022.