The National Pharmacy Association (NPA) is urging the government to use the imminent publication of the NHS 10 Year Plan to ‘turbo charge’ the role of community pharmacy after new data found that patients spent six million hours in A&E for ailments that could have been treated in pharmacies.
The analysis found that £215 million is wasted a year treating patients with minor ailments in A&E that have the potential to be safely and quickly dealt with by their local pharmacist.
Patients went to A&E with issues such as blocked noses, common colds, acne and requesting routine medication.
A reported 325,000 people alone visited A&E with a sore throat or a cold, costing the NHS £44 million in 2023/24.
The NPA has called on the government to expand the clinical role of pharmacies which would not only save the NHS money, free up A&E waiting times but also give patients quick access to healthcare professions.
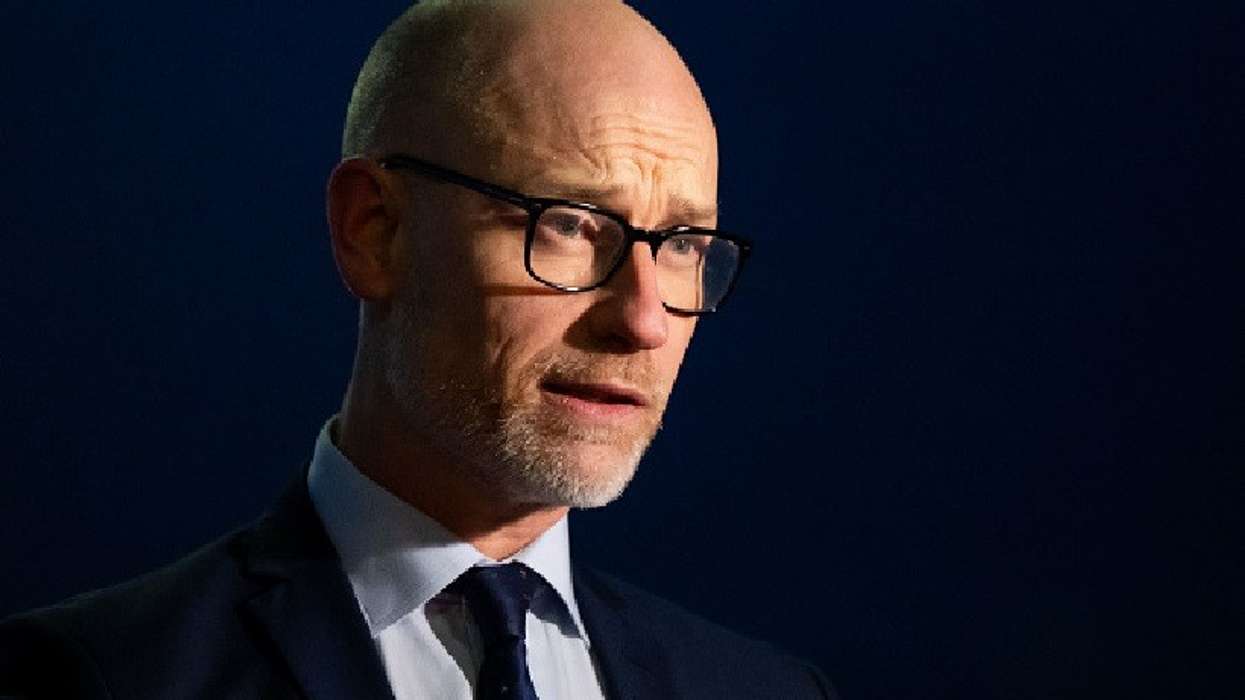
“Of course people with serious injuries should go to A&E but it should be a place for emergencies not the first place to go when faced with a minor ailment,” said Henry Gregg, chief executive of the NPA.
“Our analysis clearly shows a substantial number of visits to A&E could be better managed in a local pharmacy.
“This would be more convenient for patients, who could be treated in minutes on their doorstep and save substantial time and money in one of the busiest parts of our NHS.”
Health secretary Wes Streeting has previously said he wanted to use the 10 Year Plan to deliver a ‘transformational shift from hospital to community’.
The NPA say taking steps such as expanding the number of conditions in the Pharmacy First programme could help take pressure away from overcrowded A&E departments.
As well as this, the NPA have called for improved signposting from the NHS 111 service to direct more patients with minor ailments to their pharmacy or GP, not a hospital.
In England, pharmacists can currently supply prescription only and pharmacy medicines for seven common conditions without a patient having to see their GP, including infected insect bites, shingles and uncomplicated urinary tract infections.
The NPA are calling on the government to include additional conditions, such as constipation, diarrhoea and certain bacterial skin infections, to bring it into line with the service in Scotland.
As well as this, the NPA is calling for much greater awareness campaign for services such as Pharmacy First to encourage greater usage of pharmacy as a first port of call for certain health conditions for patients.
“The government has a once in a generation opportunity to use the 10 Year Plan to turbo charge the role of community pharmacies who, properly funded, have a vital part to play in creating a neighbourhood health service,” said Gregg.
“Investment in more clinical services in pharmacies will not only help to end the 8AM scramble for a GP appointment but also help get patients out of hospitals and into the community.
“Pharmacies still face considerable funding pressures which need resolving and investment in them is key if the government are to shift care to people’s local communities.”