By Dineshwori Longjam
With ongoing issues over funding, workforces being pushed to the limit, patient safety concerns have been growing in the UK healthcare system.
Jackie Giltrow, chair of the Community Pharmacy Patient Safety Group (CP PSG), has reassured that pharmacies remain a safe place for patients, despite the many challenges facing the sector.
"The safety culture in pharmacy is well embedded, and pharmacies are using the tools available to them effectively to ensure patient safety while continuing to deliver essential services," she told Pharmacy Business.
Martin Sadr-Kazemi, vice chair of the group and the deputy superintendent at Rowlands Pharmacy, highlighted that financial pressures are a persistent and growing challenge for pharmacies, affecting services and staff in various ways.
“Pharmacists always put patients first, making sure that they are at the heart of everything. But the growing financial pressures are creating significant challenges for the sector,” he said.
“Increased workloads, pharmacy closures, reduced opening hours, increased patient demand and medicine shortages — pharmacies are already dealing with a lot.”
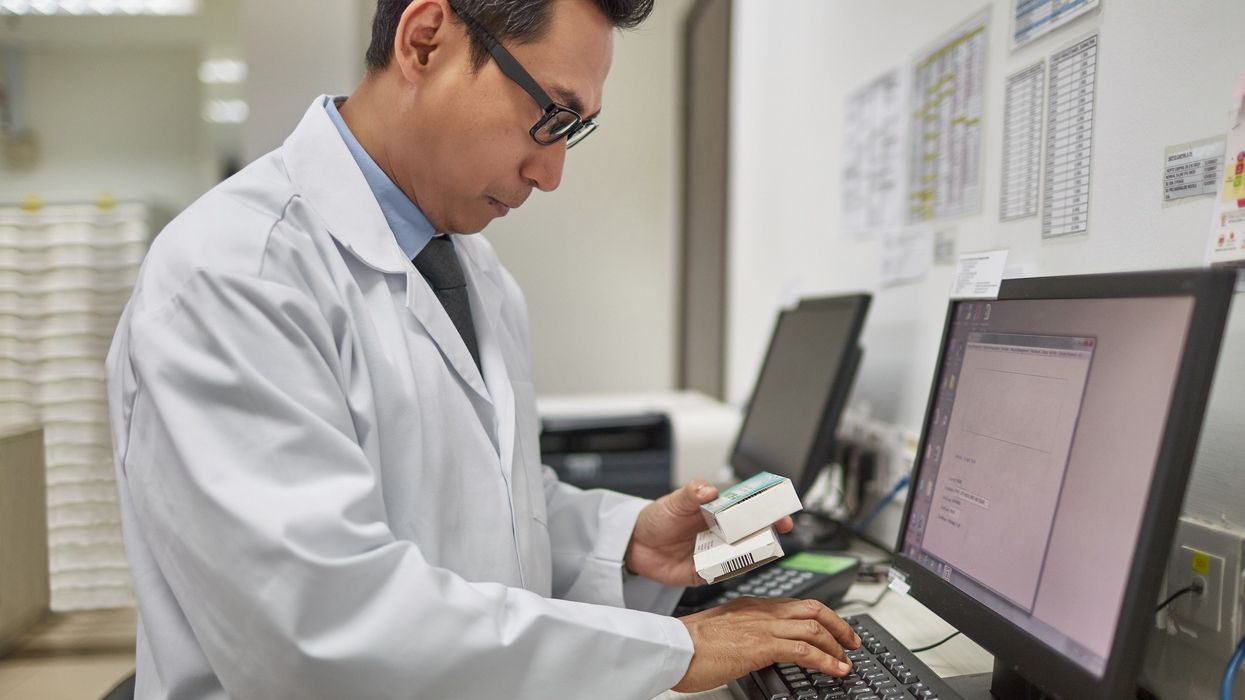
To deal with these problems, Sadr-Kazemi encourages pharmacies to focus on improving efficiencies by incorporating technology, automation, and enhanced PMR systems.
A History of Collaboration
In September 2014, NHS England and the MHRA issued a national patient safety alert recommending that all pharmacy chains with more than 50 branches appoint a Medication Safety Officer (MSO). The MSOs are responsible for reviewing medication incidents and managing safety improvements within their organisation.
To ensure full sector coverage, individual MSOs were also appointed for the National Pharmacy Association (NPA), the Independent Pharmacies Association (IPA) and Numark to support pharmacies with fewer than 50 branches.
In February 2015, these MSOs came together to form a self-funded Patient Safety Group to regularly meet, share experiences, and learn from one another. The group now meets up to 10 times annually — two of which are face-to-face meetings held in London.
“It started as a forum to share and learn. It’s still that — but it's become so much more,” said Giltrow, who is also the MSO and head of professional standards at Paydens.
The group’s role has since evolved significantly. It now engages with a broad range of stakeholders, including the Department of Health and Social Care, schools of pharmacy, Primary Care Patient Safety Strategy Group, and the valproate stakeholders group.
The Group is inviting organisations with an interest in patient safety to co-sponsor the group, and get in touch at contact@pharmacysafety.org.uk.
Key initiatives
Sadr-Kazemi and Giltrow highlighted several key areas they have been working on:
Supporting the NHS in controlled drug management
“We meet quarterly with the NHS to provide feedback and share learnings on controlled drug use,” explained Sadr-Kazemi.
Improving the labeling of children's medicines - an issue that has caused confusion and stress in both hospital and community pharmacies.
Sadr-Kazemi is part of the neonatal paediatric pharmacy MSO group, which is developing new guidelines to address this.
“We've supported the research by sending out a questionnaire to thousands of pharmacists across the Patient Safety Group network, about how we label things, and what we would do. We have reviewed the draft guidance and provided feedback,” he shared.
The guidelines are expected to be included in the Medicines, Ethics and Practice (MEP) - the Royal Pharmaceutical Society’s (RPS’s) professional guide for pharmacists, and endorsed by the General Pharmaceutical Council (GPhC).
The Group also recorded a podcast on children's medicines with the Specialist Pharmacy Service, which was very well received and shared widely across the pharmacy network.
Opioid safety
Giltrow, along with a former colleague, created a widely circulated educational video, Focus on Fentanyl, to help pharmacy teams counsel patients properly on the safe use, administration, and disposal of fentanyl patches.
“It's another piece of work we're quite proud of, and it ties in with the government's medicine safety improvement programme, especially its focus on opioid safety in non-cancer patients,” Giltrow said.
Valproate risk assessment tool
In response to new legislation on original pack dispensing, the Group created a risk assessment tool to help pharmacists make safe, consistent decisions when dispensing sodium valproate.
“The new legislation requires pharmacists to use clinical judgment to determine when sodium valproate can be dispensed outside its original packaging, and our tool ensures that everyone is using the same standard to make an evidence-based decision, keeping patients safe,” Giltrow explained.
LASA (Look-Alike, Sound-Alike) medicines
The Group worked with the Department of Health to contribute to the Pharmacy Quality Scheme (PQS), helping develop tools around patient safety reporting and risk minimisation for LASA medicines.
“These resources have had a real impact. While patient safety culture in pharmacy has always been strong, these tools have really helped teams focus on what truly matters to keep patients safe and continuously improve their practice,” said Giltrow.
The role of technology
According to Giltrow, one of the major drivers toward reducing LASA errors is automation, which she calls 'scan for safety.'
“It isn’t a panacea — it doesn’t mean there won’t be any errors — but it specifically helps prevent wrong medicine errors. When you're scanning, if you pick up the wrong box, the scanner will alert you that it’s incorrect.”
Although costly, many pharmacy chains have adopted these technologies due to their potential to improve safety and efficiency.
“Obviously, there’s a cost to implementing this technology — and it’s quite a high cost. However, many companies have decided that if you can improve safety, and gain other efficiencies too, then it makes financial sense to invest in the technology."
Sadr-Kazemi noted the benefits of robotics in dispensing at Rowlands Pharmacy: “It’s improved accuracy and freed up our teams to spend more time on the counter or in consultations with patients, relieving pressure,” he said.
Access to patient records: A game-changer
Both Giltrow and Sadr-Kazemi strongly advocate for pharmacists having access to shared patient records.
“The more information you have about someone that's relevant to their health and their well-being, the more likely you are to make the right decisions for them,” Giltrow said.
Sadr-Kazemi agreed and emphasised that as community pharmacy shifts towards delivering more services and supporting primary care, pharmacists will increasingly need access to patient records to make safe, informed clinical decisions.
“It might not make much difference to dispensing errors right now, but we're moving towards a culture where we need to start thinking about clinical errors.”
“The focus of patient safety groups will also shift as this happens, and we’ll start looking at different areas,” he added.
He also emphasised that shared records between pharmacists, doctors, and nurses would help improve communication, reduce barriers, and ultimately benefit patient care by minimizing errors and keeping processes simple.
“Patients don’t always remember everything, and we often find discrepancies between what a patient says and what their doctor has on record.
“So, pharmacists, doctors, and nurses must be on the same record — and even better, if we can access and write back. It just helps break down those barriers.”
“At the end of the day, it’s all about the patient. The more we can keep it simple, the fewer errors and issues there will be.”
Giltrow added that it also helps to ensure that the pharmacy is part of the multidisciplinary team looking after the patient.
“There are now so many services being delivered in community pharmacy — not just NHS services, but also many private ones. The more we work as part of a multidisciplinary team, the better the care will be.”
“Information is king. If you don’t have the information, you can’t always make the right decision.”
“That’s why we always tell our teams: communicate, record, and make sure records are accurately maintained on the PMR system. These records are vital for the next pharmacist or team member. If records aren’t accurate, it could give rise to patient safety incidents.”
She also stressed that it's important to record and communicate patient information accurately in PMR systems, to support continuity of care and prevent safety incidents.
However, Giltrow emphasised that pharmacists should be able to access the patient data quickly and seamlessly.
“If it takes too long or involves too many barriers—especially when you are under pressure—it’s not in the best interests of either the pharmacy team or the patients,” she said.
“It's about making sure that the pharmacists have that information at their fingertips, so they're not, scrambling around trying to find the data.”
“Pharmacists need information at their fingertips, not scattered across multiple systems, which can waste time and hinder decision-making.”
Looking ahead
With all newly registered pharmacists set to become independent prescribers from 2026, the group is already preparing.
Giltrow said that they have had discussions with the Department of Health to ensure that the right competencies are in place.
"In our organisation, we've had independent prescribers for many years, and it's that experience which will help shape how we move forward,” she added.
Giltrow also praised the collaborative ethos of the group, saying: “It's a collaborative approach, we leave any competitiveness at the door.”
“When we come into the group, it's all about patient safety — what we can learn from each other.”
"There's no secret that pharmacy teams are under pressure, but the more we can put in place to help them do their jobs safely, the closer we get to what they're really here for,” she con?
Giltrow added that while pharmacy teams are under pressure, providing them with the right support and safety tools helps them work more effectively and stay focused on their main goal—delivering safe, high-quality patient care.