Patients are struggling to access their prescriptions as pharmacies grapple with financial strain and ongoing medicine shortages.
Analysis of the ONS Health Insight Survey by the Liberal Democrats revealed that an estimated 382,000 adults visited their GP or an urgent care service in December alone because their usual pharmacy was unable to fill their NHS prescription.
In addition, a further 269,000 took no further action after they couldn’t get their prescription between 10 December and 1 January.
Overall, an estimated 3 million people—13.5% of those using prescription services—reported experiencing issues with obtaining their medication during this period.
A significant number, 426,000 people, were forced to visit multiple pharmacies to secure their prescription, while 336,000—more than one in ten affected patients—had to wait over a week to resolve their medication issue.
Furthermore, an estimated 853,000 people expressed dissatisfaction with the NHS pharmacy service they had received.
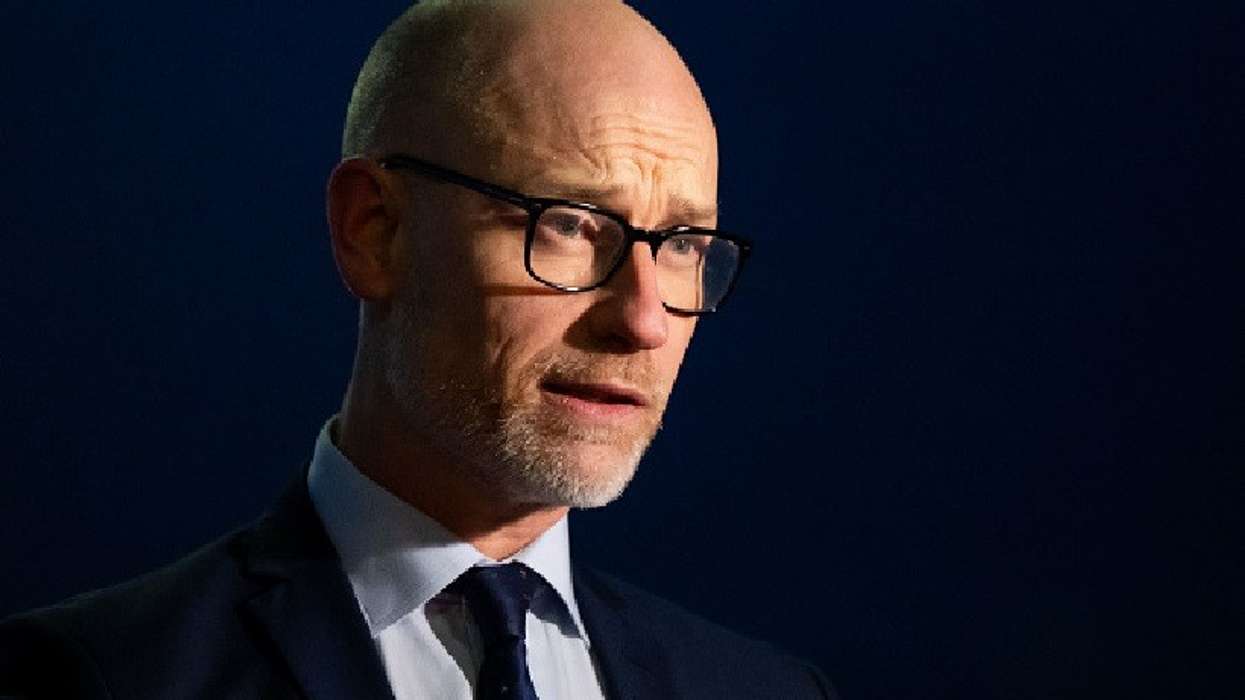
Liberal Democrat Hospitals and Primary Care spokesperson Jess Brown-Fuller MP warned that frontline health services are “at breaking point” with devastating consequences for patients.
“We have heard from countless people who are struggling to access their prescriptions when they need them with many turning to A&E or their GP or even going without the medicine they need to get through their daily lives,” he said.
“All this piles pressure on our hospitals and primary care services that are already at the brink.”
The MP accused the Conservative Party of “shameful neglect” that has punished patients in this way, and condemned the Labour government’s “total lack of urgency” as “inexcusable.”
“It is not good enough for the government to sit back and watch as people can't access the medicines they need,” he said.
He emphasised the need for urgent action to ensure “patients can access the medication they desperately need and struggling pharmacies can keep their doors open.”
The Liberal Democrats pointed to rising medicines purchasing costs as a major factor driving financial pressures for pharmacies, many of which are at risk of closure.
An analysis by the National Pharmacy Association (NPA) found that 87% of council areas have lost at least one pharmacy in the past two years.
Meanwhile, findings from the Royal Pharmaceutical Society’s (RPS) latest Workforce Wellbeing Survey paint a troubling picture of the impact of medicine shortages on pharmacy teams.
More than 6,500 pharmacists and pharmacy technicians took part in the survey, with over 40% believing that medicine shortages have put patients at risk, potentially causing worsening health conditions, flare-ups, relapses, or a reduced quality of life.
In the past 12 months, 56% of respondents reported that pressures with managing medicines shortages had directly impacted their mental health and wellbeing, and 49% said they had experienced verbal abuse due to medicine shortages.
Additional stress factors included inadequate staffing, lack of work-life balance, increased financial pressures, lack of protected learning time, lack of colleague or senior support, and long working hours.
The survey further revealed that 87% of respondents were at high risk of burnout, while only 21% felt their mental health was a priority in the workplace.
“Pharmacy teams want to do everything possible to provide the medicines their patients need, and it’s deeply distressing when they can’t,” said RPS President Professor Claire Anderson.
“This sense of ‘moral injury’ – of knowing what patients need but being unable to deliver it due to circumstances beyond their control – is taking a heavy toll on their wellbeing,” she added.
Professor Anderson stressed the urgent need for solutions, not only for the wellbeing of the workforce but for ensuring safe and effective patient care.