The Pharmacy First scheme has helped over five million patients with minor illnesses, according to NHS England.
Around 2.4 million people received help without booking an appointment at their local pharmacy for seven common conditions including sore throat, earache or shingles.
Pharmacies delivered the most consultations for acute sore throats (835,679) followed by uncomplicated urinary tract infections (UTIs) (665,409).
High street pharmacists have also delivered 1.5 million consultations for minor illness referrals and 1.4 million consultations for urgent medicine supplies.
The move means people do not have to contact their GP to receive help, freeing up appointments for those who need them most.
When Deborah, a housing manager from Stone, Staffordshire started experiencing pain and discomfort, which she believed to be a water infection, she decided to speak to her GP practice. She logged a triage form and was promptly signposted to her local pharmacy.
That same day, the pharmacy reached out to her, offering a consultation. After the consultation, the pharmacist was able to give her antibiotics to treat her urinary tract infection (UTI), and within 48 hours, Deborah felt significantly better, with her symptoms completely gone.
“Initially, I was unsure if the pharmacy could help when I experienced a painful UTI that sprung up out of nowhere. It was not something I had experienced before, but the pharmacist pinpointed the issue straight away and gave me exactly what I needed to treat it quickly,” said Deborah.
“The relief of getting fast, effective treatment, especially during a busy week, was invaluable. I had no idea a pharmacist could give prescription medication for things like UTIs without me needing to see a GP first, but the fact that they can is fantastic.”
Pharmacy First is part of a series of initiatives to offer people more choice in care close to home, ahead of the 10 Year Health Plan.
It will be expanded later this year when pharmacies will also begin offering women the ‘morning-after pill’ free of charge.
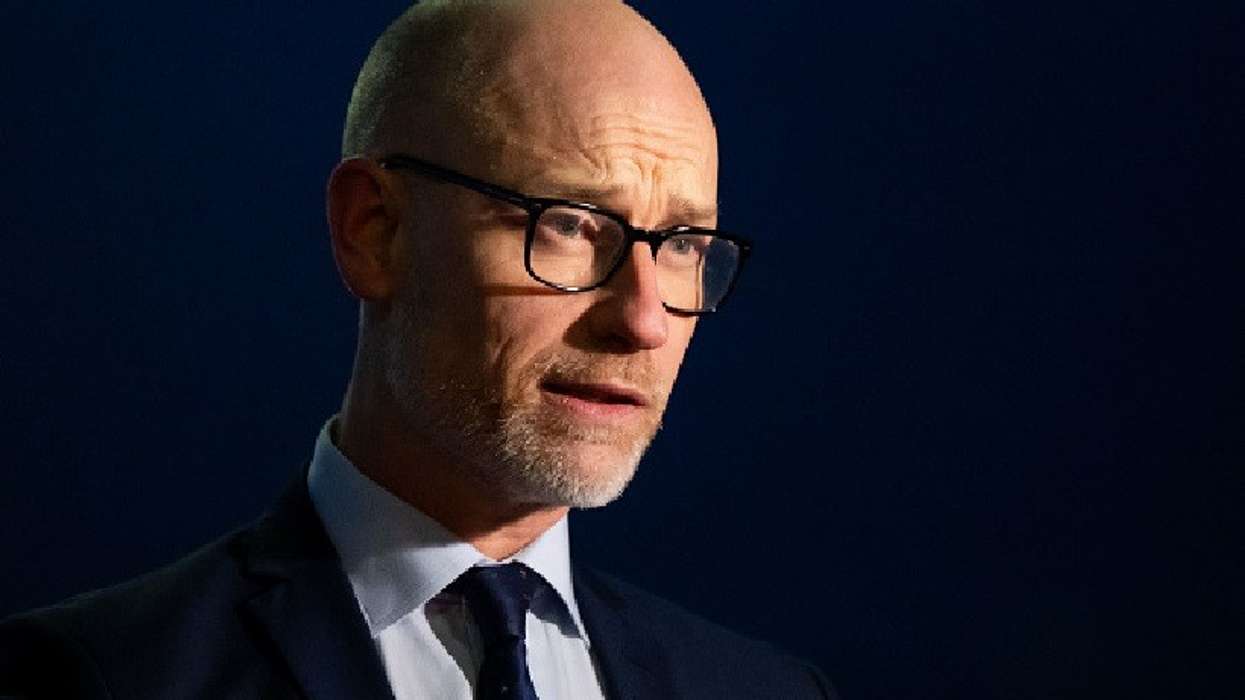
Pharmacy minister Stephen Kinnock said cases such as Deborah’s shows the impact Pharmacy First is having.
“The success stories shared by patients like Deborah demonstrate how this service is making a real difference. It is providing timely care without the need for GP appointments: a true Neighbourhood Health Service,” he said.
“I want to thank all pharmacy staff for their dedication in making this possible. As we deliver our Plan for Change to rebuild the health service, pharmacies will remain a priority, so people get the care they need close to home.”
In March, the Department of Health and Social Care confirmed it had agreed funding with Community Pharmacy England worth an extra £617 million over two years following a six-week consultation with the organisation.
A recent Ipsos Mori study showed that the public identify pharmacies as the organisation they would be most likely to go to if they needed information or advice about a minor health condition (58 per cent), but one in five (20 per cent) say they do not normally contact or visit a community pharmacy.
“I’d like to thank pharmacists, pharmacy technicians and all the staff who are employed in pharmacies for their hard work in providing high quality clinical advice and care to more than five million people,” said David Webb, chief pharmaceutical officer for England.
“Pharmacy is a critical element as the shifts NHS care from hospitals to the community, treatment to prevention, and analogue to digital.
“The 78,000 registered pharmacists and pharmacy technicians in England are skilled professionals who operate in the heart of the NHS and their communities and are highly trusted by the public.
“The recent additional investment underscored the importance of community pharmacy as an integral part of the NHS team, providing clinical care, optimising the use of medicines and supporting people in their neighbourhoods to prevent ill health.”